Cervical Disc Herniation
05/05/2022
最終更新日時 :
03/10/2024
 webmaster
webmaster
We will provide information on the surgical methods for cervical disc herniation, the length of hospital stay, and whether the procedures are covered by insurance.
Cervical Disc Herniation
What is Cervical Disc Herniation?
Just like the lumbar spine, the cervical spine has intervertebral discs between the vertebrae. These discs function as cushions and allow mobility in the spine. Due to aging or other factors, cracks can develop in the surrounding annulus fibrosus, leading to the contents of the disc protruding and causing a cervical disc herniation.
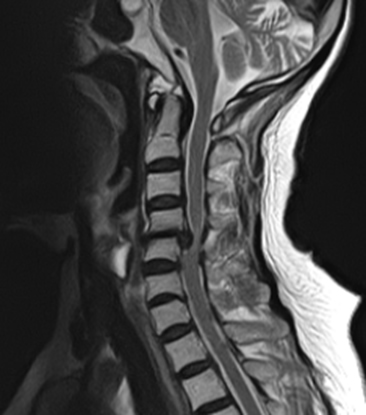
Symptoms
The symptoms of a cervical disc herniation vary depending on the direction of the protrusion. If the herniation compresses the spinal cord itself or the nerve roots (branches of the nerves) that branch off from the spinal cord, it can cause pain and numbness on one side of the neck, shoulder, shoulder blade, and arm, along with possible muscle weakness. On the other hand, if the herniation protrudes significantly towards the center, it can compress the spinal cord itself, leading to difficulties with fine motor movements of the fingers, walking difficulties, and bladder or bowel dysfunctions (such as frequent urination, urinary retention, or incontinence).
If severe pain or numbness does not improve with conservative treatment or if neurological deficits due to spinal cord or nerve root compression occur, early surgical intervention may be required. If you experience symptoms like those described above, please consult a specialist in spinal disorders.
Surgical Methods
Surgery is broadly categorized into two methods based on the size and location of the herniation compressing the spinal cord:
Anterior Approach (Anterior Decompression and Fusion): This method involves accessing and treating the herniated disc from the front of the neck.
Posterior Approach (Posterior Decompression): This method involves accessing and treating the herniated disc from the back of the neck.